By ICHP Executive Director, Jonty Heaversedge

At ICHP we are proud to support the North West London health sector in its journey towards a model of care driven by actionable insights from real-world evidence. The potential for systemic use of data is huge: From enabling us to risk stratify patients so that those in greatest need are proactively prioritised (Population Health Management); to delivering more equitable care by reallocating resources to those with the poorest outcomes who are most disadvantaged by current care provision (Core20+5); to helping us reduce variation in care quality by helping professionals adopt best practice and optimise care (Clinical Effectiveness). There is no denying smarter use of data is an exciting prospect.
But for real impact to be delivered for our population through the use of data, we must be both systematic and systemic in our approach, and this does not come without challenges.
In my experience, NWL colleagues, but particularly community pharmacists and GPs, like me, are excited by the prospect and recognise the value of data. After all, we have always felt a deep connection to the communities we serve and prided ourselves on trying to stay up to date with the latest research and evidence – ensuring our patients receive the best possible care. So additional data and insight that enables us to do this more effectively is a good thing for us all. But data and insight are inherently about understanding opportunities for improvement. There is no getting away from the fact that benchmarking using data can help us identify opportunities for improvement, but when you have a strong vocation, very little about analysing your performance doesn’t feel personal.
There is no denying smarter use of data is an exciting prospect. But for real impact to be delivered for our population through the use of data, we must be both systematic and systemic in our approach.
Then there is the practical challenge: how do health professionals adopt data-driven insight into their day jobs with all of the pressures they are facing? It is often just another thing to do in an already busy consultation, and time, as we know, is incredibly scarce in primary care at the moment.
This is linked to a wider cultural challenge: General practice has always prided itself on providing continuity of care from cradle to grave, but over time the demands it has faced have resulted in care becoming more reactive and opportunistic, and dependent on the patient identifying a problem and seeking help. So, even if reviewing data and insight in itself isn’t a massive change, using data to offer more proactive or preventative support requires quite a fundamental change in culture, new ways of working, and will feel like an additional demand on an already busy practice team.
All of these challenges make working collaboratively even more imperative. By sharing priorities and resources, and creating a system-wide culture that highlights variation as an opportunity for learning and not criticism. By all pulling in the same direction with one specific focus, we will see Impact, on our population more quickly, which will help energise us all too. So how do we move from theory to action, together? Or, to coin a phrase used at our previous NWL Clinical Effectiveness meeting, pinched with pride from colleagues south of the river, how do we make ‘the right thing to do, the easy thing to do’ for us all? The infamous Desmond Tutu quote comes to mind: One bite at a time.
Focusing on case finding allows us to not only generate the insights and partnership to deliver the work, but also create the right conditions for success and shared learning.
And that’s where the Big NWL Case Find: Hypertension hopes to come in.
So how do we move from theory to action, together? Or, to coin a phrase used at our previous NWL Clinical Effectiveness meeting, pinched with pride from colleagues south of the river, how do we make ‘the right thing to do, the easy thing to do’ for us all?
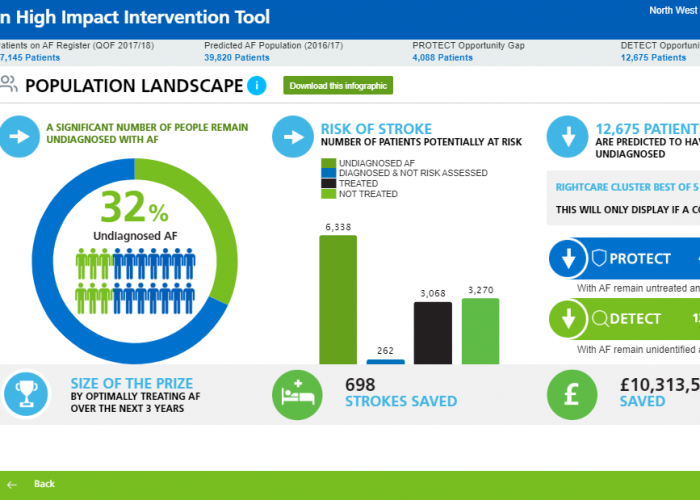
As a NWL primary care system we are using the month of May to focus on just one thing: detection of hypertensive cases. We have an 83,000-prevalence gap in hypertension in North West London, compared to expected cases. That’s 83,000 people who are all at risk of an adverse CVD event if we do not get their hypertension managed. Detection is the first step.
The Big NWL Case Find aims to detect some of these ‘missing’ cases by asking Primary Care colleagues to perform blood pressure checks at every clinically appropriate patient contact, to review WSIC and ensure that patients are properly coded, and – where relevant and able – to deliver additional blood pressure check clinics. By focusing on this first phase of pathway optimisation, we’re hoping to get a more accurate picture of what’s going on in the whole system so that we can then prioritise the work that we must do to have greatest impact as a whole sector.
Focusing on case finding allows us to not only generate the insights and partnership to deliver the work, but also create the right conditions for success and shared learning. It also sets us up to be able to collectively focus on the next part of the pathway, with more knowledge and understanding to inform action.
Supporting the transformation of NWL into a learning health system and transitioning to a more proactive and personalised model of care is possibly the most important thing we can do in our lifetimes. But equally important is ensuring that we do it together.
To get more information about the Big NWL Case Find: Hypertension, email cardiovascular@imperialcollegehealthpartners.com.