 Andi Orlowski, ICHP’s Head of Business Intelligence, discusses why the obvious answer may not always be the best answer when it comes to population health….
Andi Orlowski, ICHP’s Head of Business Intelligence, discusses why the obvious answer may not always be the best answer when it comes to population health….
In medicine, ‘Sutton’s Law’ is the principle of going straight to the most likely diagnosis, or the most obvious answer. While this may make sense when it comes to clinical decision-making at an individual level, this way of thinking may trip up those involved in the wider issue of population health.
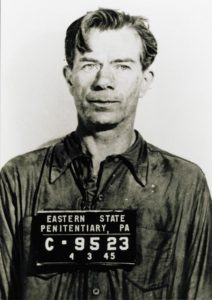
The ‘law’ is usually attributed to US bank robber Willie Sutton, also known as ‘Slick Willie’. Although caught on a number of occasions, Willie escaped over and over again to continue his criminal career, stealing an estimated $2 million. At one point a reporter asked him why he kept on robbing banks and his simple answer was supposedly “because that’s where the money is”. Obvious, right?
However, when integrated care system (ICS) managers start working with population health analysis they should be wary of Sutton’s Law, as the obvious answers or new ways of working may not always be the most cost effective options or the ones that serve local people best. (Find out more about population health assessments in our blog ‘Know your audience’.)
Assessing the needs of a population
One of the first steps in working with population health is carrying out a needs assessment, which ideally involves ICSs working with local authorities and public health as well as primary and secondary care NHS teams and data.
This needs assessment should identify the health and care needs of local people and important segments within the population. These segments can then be compared to peer matched populations to see, through unwarranted variation and other analyses, where there are opportunities to improve health.
And this is when Sutton’s Law can start to play a role – and where specialists in population health analysis can help keep resources targeted appropriately.
How impactibility considerations may offset Sutton’s Law
Say, for example, there is a segment with a relatively small population that has a high risk and large associated healthcare costs. There is also another segment with similar levels of risk and costs, but a large population.
Sutton’s Law would suggest the easiest opportunity to make an impact would lie with the segment including the fewest people – the thinking being that with fewer people to direct an intervention at, this appears an obviously more efficient use of resources.
However, while this first segment might be responsible for a disproportionate number of admissions or costs, it is not responsible for the majority of admissions. The greatest reduction in admissions could come from reducing the risk to the second, larger segment of the population.
In addition, targeting the highest risk segment of the population may look like an obvious place to start, but those individuals may already be well known to healthcare services and already receiving optimised care. Trying to add extra interventions for someone who has maximised healthcare could lead to little or no gain (diminishing returns).
Measuring impactibility
Once we have completed an opportunity analysis to identify potential areas for improvement for all segments of the population, at ICHP we follow up with a look at impactibility – identifying which patients are most likely to be amenable to an intervention and which interventions would be most effective.
When looking at the patients themselves, we can use predictive analytics or risk scores to help predict individuals who are at high risk of developing disease or suffering an adverse event. We can also look at gaps in care, where we search for patients who may not have been offered an intervention or who may benefit from stopping one, and find patients who have not yet received appropriate tests, education or advice.
When considering interventions, we look to see that they are appropriate for the population highlighted in the potential opportunity. We carry out a literature and case study review to see whether an intervention has been used in a similar population and, if it has, what the outputs and outcomes were. We can then consider how that intervention might translate to the target population.
By focusing on impactibility, we can help decision-makers address health inequalities and consider the ethical impact of planned interventions by ensuring new interventions are targeted at those at risk of poor health outcomes whose needs aren’t currently being met, and not those who already have optimal support for their condition.
And by helping managers better understand the opportunities in front of them and sometimes demonstrating that following Sutton’s Law of going for the obvious isn’t necessarily the best answer, we can also ensure precious resources are targeted in the most effective ways.
Here’s some further reading on the topic that you might find useful:
Dr Geraint Lewis, Next Steps for Risk Stratification in the NHS – NHS England website