Andi Orlowski, Deputy Director of Business Intelligence, explains why value isn’t about what you can measure, but what you should measure.
Traditionally in the NHS we’re used to thinking of value as value for money. However, as we now look to address the wider determinants of health with an integrated system approach there are potentially other ways to measure value – care outcomes and user experience for example.
This is the difference between cost benefit models, where the outputs were always in financial values, versus cost effectiveness or utility models, where we look at incremental gains in health and quality of life.
As integrated care is further developed across England, how we offer value is no longer a discussion that individual organisations have internally, it’s a conversation that health leaders are having across whole systems.
A recent event hosted by Imperial College Healthcare focused on this issue, looking at how we can start building business cases that focus on best possible value, utilising population health data and new ways of measuring value to help support decision-making.
What is best possible value?
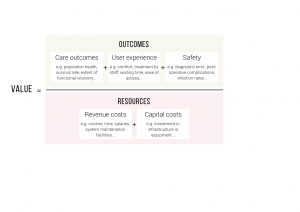
At the event we discussed a model (the Future Focused Finance Best Possible Value Framework) where value equals the outcomes (care outcomes, user experience and safety) divided by the resources (revenue costs and capital costs).
The most interesting part came when the attendees were given a commissioning decision to make on a fictional change to services, and were asked to come up with which criteria and metrics should be used to measure the value. This turned the usual way of thinking on its head, challenging people to think of, for example, what kind of patient experience criteria we should use and how to measure them, rather than simply looking at what data we already have available and using that.
A model like this challenges us to think about what matters and then measure it, not just think about what we can count. In addition, under this model, to get the best possible value, you must improve outcomes or reduce resources without compromising either, and conceptualising value in this way provides a single uniting goal and a common language for both finance and clinicians to speak.
A culture of value and improvement
With the increase in integrated care, we need to work together to make decisions, using fixed resource across the sector and shifting money across traditional boundaries. Conversations are already being held at executive levels around the country about value and improvement, with the concept being embedded through strategic objectives.
Developing a values-based business case and evaluation can be difficult as criteria such as patient experience can be trickier to measure, and we need an agreed framework for doing that, so we can make consistent decisions.
We recently worked with Hillingdon CCG to look at how their spend on falls is broken down, and our analysis showed that around half of the population health gain from interventions came from 95 per cent of the money spent (hospital admissions). This means that the other half of the benefit to patients was gained from just five per cent of the spending – mainly on preventative interventions that reduced the risk of falls. However, the transfer of funds to the preventative interventions has to be structured to ensure the hospital remains sustainable.
So a balance still needs to be struck, and values-based decisions can help with this. Dominique Allwood (consultant in public health medicine and associate medical director QI at Imperial Healthcare and assistant director of healthcare at The Health Foundation) gave as an example the issue of funding interventions that tackle wider health issues, such as Redthread, a hospital based youth violence intervention delivered in emergency departments. These types of service tend to be run by voluntary and third sector organisations but they sometimes struggle to complete a traditional business case as the value they add is often at a wider societal level, or preventative benefits such as onward reduction in harm, and the benefits are seen over a much longer time period than a funding cycle.
Dominique said that developing a values-based business case would mean they could evidence the value that extends beyond the organisation itself. She said: “NHS organisations are being encouraged to work more closely with each other and beyond with social care and with others, so decision-making is no longer solely down to individuals and organisations in isolation. Values-based approaches tend to push you to think more broadly about costs incurred and where impacts are felt and over what time.”
Dominique also highlighted a topic close to my heart after the event, about the importance of data in supporting value-based decisions. She said: “Organisations are very good at collecting data that relates to their organisation, but how do we collect those outcomes that span whole places, when people haven’t yet thought through what that means? That’s where the outcomes-based conversations need to be happening, at the level of integrated care systems.”
This is a discussion that I hope will be being mirrored in integrated care systems across the country, as we all grapple with new ways of commissioning that recognise the value of what we provide, and the new interdependence of health and social care. Please do let us know if your ICS is having similar discussions and you’d like to share your thoughts on how we can make value in public health a key component of how we commission care across whole systems. Email Andi Orlowski, Deputy Director of Business Intelligence at andi.orlowski@imperialcollegehealthpartners.com.