Ralphael Oghagbon, Health Economist, outlines the benefit of a STAR analysis when evaluating the cost and value of different interventions on a patient pathway across a whole health system.
With an increased focus on integrated working across health systems, ICHP’s evaluations of services and treatments are increasingly being called on to look at whole patient pathways rather than individual interventions.
To support this wider visualisation of a care pathway, we’re starting to work with a new type of analysis that looks at the socio-technical allocation of resources (STAR). It involves measuring the allocative efficiency or the effectiveness of spend across a whole pathway and enables CCGs and integrated care systems to consider whether a reallocation of resources could lead to better patient outcomes.
Pulling together a STAR analysis involves a high level of collaboration, with the shared knowledge and experiences of commissioners, providers and patients all playing a part in demonstrating the relative cost and benefit of each intervention along an entire patient pathway.
How a STAR analysis works in practice
As I write, we’re in the final stages of our first ‘live’ STAR analysis, which was requested by Hillingdon CCG to assess its pathway for falls and falls prevention. In carrying out the work, we’ve called on the expertise and previous experience of Senior Project Manager Richard Glover from one of our partners, the North of England CSU.
Our first step was to work with the CCG to identify and meet with the key stakeholders so that we could get everyone involved in the process – including primary care, secondary care, social care, community providers including Age UK, those supporting recovery such as physios and day care, and the patients themselves.
We pulled data from published articles and NICE as research on what pathways should look like before we then invited representatives from all these groups to a workshop. At the workshop we asked the participants to work in groups to describe the current pathways and their thoughts on how they work, and to share their experiences of those pathways and ideas on what an improvement could look like. The aim was to share experiences and identify how the pathway was working in reality with a focus on patient-based outcomes.
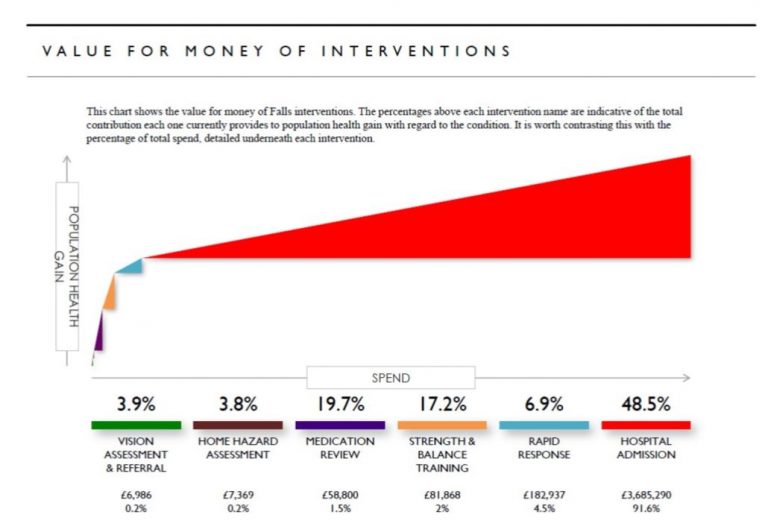
Following the workshop we used the STAR tool to analyse the information we had gathered coupled with data on the pathway from the CCG. The tool generates a graphical visualisation that includes triangles representing each intervention on the pathway, allowing us to see how much is being spent on each one and relatively how many people benefit. The approach helps stakeholders compare interventions, assess their value for money and better informs return on investment which is an important consideration for decision makers tasked with providing care for a population with finite resources. We held a second workshop around a month later with the same group. This time we shared our mapping of the pathway and outputs from the STAR tool and had a conversation about the local picture and how it compared with national guidelines, to stimulate discussions amongst stakeholders about how it could be improved.
The feedback from the second workshop will be included in our final report to the CCG, which will cover the high level data and give suggestions on moving forwards, including small changes that the stakeholders agree should be possible.
The whole process is designed to stimulate discussion on what could be done to improve the pathway in a region. By considering societal benefit and the importance of prevention, it’s possible to rebalance the funding of healthcare to better suit the needs of the population and ensure that money is spent in the best way to address a health problem.