The NEWS2 (National Early Warning Score 2) tool allows a patient to have the acuity of their condition assessed quickly and objectively so that they can be triaged and escalated to the appropriate clinicians or services, as well as increasing the likelihood of sepsis being detected sooner. Imperial College Health Partners (ICHP) have been working with intermediate care services in Northwest London to roll out an easy-to-use NEWS2 app, created by the Royal College of Physicians.
NEWS (National Early Warning Score) is a tool which helps clinicians identify acutely ill patients, and NEWS2 is the updated version released by Royal College of Physicians in 2017.
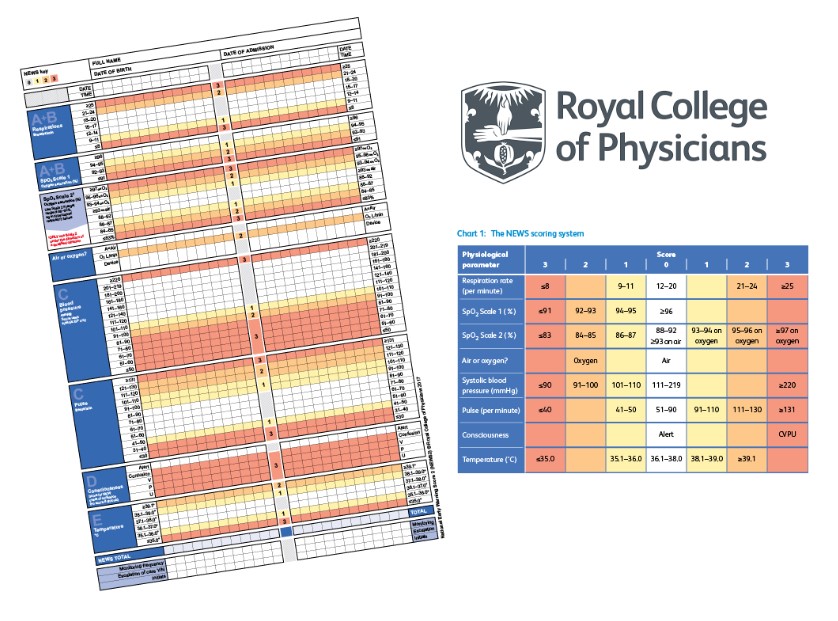
The scoring system takes the six simple physiological measurements, routinely recorded during clinical assessment, and allocates a score to each. The higher the aggregated score, the more extreme the variation from the norm and more unwell the patient. An accompanying escalation protocol guides the clinician on how to act.
In 2019, an app was launched by Royal College of Physicians to improve accuracy of score calculation.
Up until most recently, early warning scores have been mainly used in secondary care however we are fast learning the value of having a standardised tool across all settings to better detect and communicate the deterioration of patients.
In North West London, whilst all secondary care providers are using NEWS2, most intermediate care services are not. As a result, ICHP sought to support the spread of NEWS2 across all settings by starting with its introduction, facilitated by the app, into two intermediate care services – CLCH Walk-In Centres (5 in total) and LNWUHT Rapid Response team.
This project aimed to incorporate NEWS2 into each service’s clinical assessment.
The first task was to understand how a scoring tool, most commonly used in acute care, could be translated into each intermediate care service. Engagement began with both teams around March 2018. This included running workshops with clinical leads to map each service processes. These workshops, supported by baseline data, were used to identify the size of the opportunity and relevant patient populations. Each escalation protocol was co-designed with the services to ensure that guidance matched available resources and the experience of team members. All changes and decisions were fed through a steering group facilitated by ICHP, who also decided how staff would be trained, how the project would be evaluated and ultimately sustained.
For both teams, a phased approach was taken for implementation. Clinical leads of each service began by systematically rolling out NEWS2 training for staff members before launching. Users were trained on the principles, the escalation protocol and the app. In parallel, access to the apps was made via clinic desktops (CLCH) or through smart devices (STARRS team).
Interim meetings held with clinical leads were used to troubleshoot difficulties. Bringing together clinical leads on a regular basis provided a forum for sharing ideas, sounding out solutions and reflecting. These meetings were key when CLCH began trying to understand how NEWS2 scoring could be integrated into its electronic records and when sharing resources and lessons learned for training staff. Where possible, ICHP helped to articulate the problem and facilitated discussions to find solutions.
At the end of March 2019, the Rapid Response team of STARRS were trained in and using NEWS2 as part of their routine clinical assessment. By the end of June 2019, all 5 Walk-In Centres in CLCH had reached the same point.
As a result of this project, both teams have readily adopted NEWS2. Despite never using scoring systems before, both teams had fantastic engagement from staff and clinical leads received positive feedback about its use in supporting clinical decision-making as well as for communicating deterioration to other clinicians.
The STARRS team calculated NEWS2 scores in 93% of all patients reviewed after 1-month of implementation, increasing to 97% when evaluating at 3 months. This showed incredible staff engagement from a service that sees up to 400 new patients a month. Following implementation, patients were more likely to have all observations taken and be escalated appropriately as a result.
Despite seeing much smaller numbers of acutely unwell patients, there was still good adoption of NEWS2 by CLCH Walk-In Centre staff. NEWS2 scoring was performed in 80% of emergency transfers and staff instinctively began incorporating the score into day-to-day language. For example, when handing over to LAS, paramedics could easily understand the urgency of a patient with a “NEWS of 7”.
The next steps are to improve sustainability and to spread NEWS2 into other teams. Firstly, each team has identified small changes that could be made, e.g. introducing a training log for agency staff, which may further improve the integration of NEWS2 into their day-to-day practice. ICHP will support the evaluation of these changes using QI methodology. Secondly, both clinical leads also work closely with District Nursing teams. Spreading to District Nursing would be a natural next step and ICHP will be supporting these teams going forward.
“CLCH walk in centres and urgent care have worked together with ICHP to implement NEWS2 scoring to adults attending with urgent illness conditions.
“This has been really well received by clinicians across the centres to improve recognition of deteriorating patients. Staff found a language developing to standardise communication and prioritisation amongst the team and to the multi disciplinary team they are referring to including ambulance trusts and secondary care.
“Completing the score using a tool embedded in the clinical system and use of an adapted escalation tool has led to improved patient safety and prioritisation. It has also allowed teams to evidence acuity and complexity of attending patients and facilitate their on going referral if needed to a standardised pathway.”